Trauma-Informed Considerations of Restrictive Practices for Essential Treatment & Care – Part 2: Action Steps
As a follow-up to a previous post, in this one, we will consider the key principles of trauma-informed practice and suggest practical ways in which you can avoid some of the potential factors adding to trauma when deciding upon the suitability of the use of restrictive practices to deliver treatment safely.
Trauma-Informed Practice
There are currently lots of definitions of Trauma-informed Practice. Here, we are using one that is contained within the Trauma-informed Practice Toolkit -Scotland, which we highly recommend as a great resource for staff and arguably show the rest of the UK how it should be done.
Trauma-informed Practice
A model that is grounded in and directed by a complete understanding of how trauma exposure affects service user’s neurological, biological, psychological and social development.
Scottish Government. (2021). Trauma-informed practice: A toolkit for Scotland.
https://www.gov.scot/publications/trauma-informed-practice-toolkit-scotland/documents/
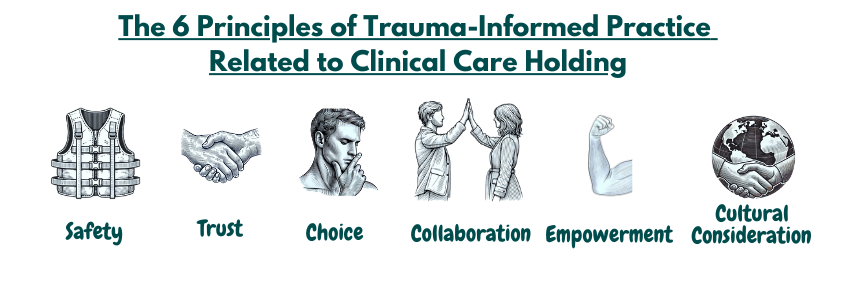
Using this as a foundation to build practice on and structure your approaches using the six principles of Trauma-Informed Care will give a good framework for identifying and delivering practical actions during times when restrictive practice in its’ many forms may have to be used to deliver serious medical treatment or essential care practices.
The 6 principles of trauma-informed practice are :
Despite having this approval and knowing that the procedure or serious medical treatment is in the person’s best interest, staff, parents, and carers must still ensure that as many measures as possible are in place to reduce the likelihood of trauma occurring.
These 10 potential factors identified were
-
-
- Communication Barriers
- Previous Experiences
- Lack/Loss of Control
- Physical Discomfort
- Nature of the Procedure/Test/Treatment/Care
- Post-Treatment Care
- Frequency of Treatment
- Presence of Family Members / Others
- Staff Confidence and Training
- Environment
-
Clinical Holding and Trauma-informed Practice
If we relate the 6 Key principles of trauma-informed practice above to these 10 highlighted factors, then it allows staff and/or parents and carers to identify some action points to consider.
To promote safety, staff should focus on creating a calm and non-threatening environment and offering clear and simple communication. In most settings, this will already be part of an ongoing relationship-building process that also enhances communication. A crucial element of staff behaviour, before, during and after the treatment or procedure, is that they remain alert and provide immediate and ongoing emotional support. This is fundamental, and what this will look like should be discussed during the planning and training stages.
It is crucial to train staff to handle procedures confidently and compassionately. Some organisations feel that staff who have had “Restraint Training in Managing Violence & Aggression” or because they are “Security Staff” and it’s “their job” are trained for such procedures, but rarely is this type of training focussed or relevant to these situations. Holding people supportively for clinical care procedures requires additional considerations and has completely different learning outcomes and goals.
Additionally, linked to good communication, staff can address safety by having effective strategies and tools in place to help assess any potential physical discomfort caused by the medical treatment or care procedure. Identification and prompt, effective responses to pain and discomfort must always be a key consideration from the initial best-interest discussions and meetings. The ability for the person to communicate they are experiencing pain may need specialist input from a speech & language therapist.
 A key value held by caring professionals and organisations is that of trustworthiness, which comes through transparency and can be initially seen in the organisation’s policies and procedures. However, despite what is written down, how this translates into actions is really all the supported person is concerned about. Equally, staff have to feel the organisation is transparent and trustworthy with them. This is important when staff need confidence and feel safe to truly support the vulnerable patient during the procedure.
A key value held by caring professionals and organisations is that of trustworthiness, which comes through transparency and can be initially seen in the organisation’s policies and procedures. However, despite what is written down, how this translates into actions is really all the supported person is concerned about. Equally, staff have to feel the organisation is transparent and trustworthy with them. This is important when staff need confidence and feel safe to truly support the vulnerable patient during the procedure.
Building trust is a continual process and is achieved by consistently providing reliable information about procedures, ensuring that the patient understands what to expect, and following through on promises. Everyone has a friend with horror stories about when the dentist didn’t stop as agreed during treatment. Whether true or otherwise, this demonstrates the vulnerability everyone feels at such times.
Clearly explaining the steps involved in care and involving patients and their families in the process can further enhance trust. Regular communication and transparency in decision-making are essential to fostering a trustworthy environment.
 Treatment enabled through the use of Clinical Care Holding procedures can appear as a contradiction when considering choice. It may be seen as taking away choice when the person is dissenting to the treatment, and it continues. It has to be remembered (and as discussed in length elsewhere on this website) that it will only sometimes happen after the Court of Protection has authorised it.
Treatment enabled through the use of Clinical Care Holding procedures can appear as a contradiction when considering choice. It may be seen as taking away choice when the person is dissenting to the treatment, and it continues. It has to be remembered (and as discussed in length elsewhere on this website) that it will only sometimes happen after the Court of Protection has authorised it.
However, there are still lots of important opportunities and plenty of ways in which the supported person can express choice, and staff need to respond mindfully to these so they are included in the treatment plan.
This includes allowing them to decide on aspects of their treatment, pre-medication, pain management, presence of family members or significant others, for example. Depending on the treatment or procedure, other considerations such as time of day, location, toy, music, etc, can be decided by the person where they are able. Encouraging the supported person’s input and respecting their decisions reinforces their autonomy and engagement.
Staff should be reminded that while they may have legal authority to proceed with the treatment, they must not deny the person’s autonomy in anything else they are able to choose for themselves.
One last consideration for trauma-informed organisations is their staff members’ choices and making provision for them to “opt-in” to participate in the treatment/procedure. Sometimes, staff have very good reasons why they are not the best person to support or present during such scenarios.
 Arguably, healthcare worldwide, but certainly within the UK & Ireland, could not function without the input, help, support and collaboration that families and carers give during times of treatment and care procedures. It should be assumed that staff continually seek to work collaboratively with the people they support, and within intellectual disability services has always been a foundation keystone.
Arguably, healthcare worldwide, but certainly within the UK & Ireland, could not function without the input, help, support and collaboration that families and carers give during times of treatment and care procedures. It should be assumed that staff continually seek to work collaboratively with the people they support, and within intellectual disability services has always been a foundation keystone.
Collaboration can be fostered by involving the person and those important to them in discussions about their care and proposed treatment and looking for their feedback to improve practice.
Encouraging a team approach among staff and individuals they support ensures everyone’s experiences and insights are valued.
Real person-centred approaches that focus on “doing with” rather than “doing to” should be ingrained in organisations, and serious medical treatment or care procedures require staff to be extra vigilant of this in their practice.
 Where it has been identified that there may be a potential need to use a restrictive practice to deliver treatment, the organisation needs to be able to demonstrate how it has worked collaboratively to share power and give both the supported person and also the staff a strong voice in the decision-making process.
Where it has been identified that there may be a potential need to use a restrictive practice to deliver treatment, the organisation needs to be able to demonstrate how it has worked collaboratively to share power and give both the supported person and also the staff a strong voice in the decision-making process.
Empowerment involves continually educating individuals in their care about their options and involving them in every step of the process. This can be achieved by supporting self-advocacy, encouraging people to make informed decisions, and providing resources to enhance their understanding. This may include the need to involve other professionals for their speciality help and input, such as psychology services, speech and language services or occupational therapy, for example. Not simply relying on the knowledge and skills of the in-house staff team.
Strategies are essential to make parents and carers feel like they have a voice in the procedure and that they are listened to.
Finally, empowering staff to feel confident to deliver the treatment and to support the person through this potentially fraught situation. This is achieved through continuous training and professional development and regular meetings where they are supported to voice their opinions or any concerns. This helps ensure that they can effectively support and advocate for the supported person.
 Understanding and incorporating cultural, historical, and gender contexts is essential in trauma-informed care. Staff have a duty of care to demonstrate effective cultural competence and take into consideration the person’s cultural beliefs, values, and practices, as well as those of their families. Organisations and staff may consider enlisting the help of cultural brokers and community health workers who can offer guidance and education to the staff team that is relevant to the individual they are supporting.
Understanding and incorporating cultural, historical, and gender contexts is essential in trauma-informed care. Staff have a duty of care to demonstrate effective cultural competence and take into consideration the person’s cultural beliefs, values, and practices, as well as those of their families. Organisations and staff may consider enlisting the help of cultural brokers and community health workers who can offer guidance and education to the staff team that is relevant to the individual they are supporting.
Recognising and respecting cultural, historical, and gender contexts can significantly reduce the likelihood of trauma and improve the overall care experience.
Historically, people in supported environments may have already been exposed to poorly executed clinical treatment by professionals who may have appeared uncaring to them. These historical incidents and their associated memories may not be known by staff in the current service. Therefore, it is important staff seek to find out from those close to the individual if there may be any significant indicates they need to be mindful of when planning.
Incorporating this knowledge of historical contexts into the treatment plan may help avoid re-traumatisation and build trust.
Summary
Health and Social Care professionals are responsible for putting strategies in place to avoid causing trauma to people in their care. Taking time to consider this at all aspects of the planning and training stages is paramount.
Action Points for Staff Include
Safety: Ensure a calm, non-threatening environment and provide clear, compassionate communication to promote safety during treatment.
Trust: Build trust by consistently offering reliable information, involving the person and families in decisions, and demonstrating transparency in actions.
Choice: Empower the person by allowing them to make choices in their treatment and respecting their decisions wherever possible.
Collaboration: Foster a team-oriented approach by actively involving the individual, families, and staff in care discussions and decision-making processes.
Empowerment: Support self-advocacy and informed decision-making by educating individuals and staff and involving them in every step of the treatment process.
Cultural Consideration: Respect and incorporate cultural, historical, and gender contexts to enhance understanding and reduce the risk of trauma.
By integrating these six key principles into their practice, staff can significantly reduce the likelihood of trauma and ensure a supportive, empathetic, and effective care environment for individuals who lack capacity.